Clinical trials research the way a drug or treatment will interact with the human body. There are currently thousands of different gene and cell therapies being studied in clinical trials in hopes there could be a potential treatment for diseases that have little to no other treatment. Learn more about preclinical studies, the phases of a clinical trial, how to find a clinical trial, and FDA efforts to make the process faster.
Before a Clinical Trial
Preclinical studies happen before a clinical trial starts. These studies test the treatment in cells or animals. The goal is to find out if the treatment will work and how much of it is needed (dosage) to see a positive effect. It also tests the safety by looking for any negative effects. If the preclinical results are promising, meaning it provides a participant with more benefit than risk, the researcher will design the study for humans.
.aspx?width=350&height=350) Investigational New Drug (IND) application is how the preclinical study data and clinical trial design are submitted for review to a government regulatory agency. In the United States this is the U.S. Food and Drug Administration (FDA). The FDA, working alongside local ethics committees, reviews the information and data to make sure the researcher has done everything possible to minimize risks to the potential study volunteers. Once the FDA agrees that risks to volunteers are minimized, a clinical trial can begin.
Investigational New Drug (IND) application is how the preclinical study data and clinical trial design are submitted for review to a government regulatory agency. In the United States this is the U.S. Food and Drug Administration (FDA). The FDA, working alongside local ethics committees, reviews the information and data to make sure the researcher has done everything possible to minimize risks to the potential study volunteers. Once the FDA agrees that risks to volunteers are minimized, a clinical trial can begin.
Eligibility criteria are characteristics that all participants must have. For every clinical trial there are set rules for who can and cannot participate in the study, also called inclusion and exclusion criteria. These commonly include age, gender, specific gene variants, medical history and more. By making sure that volunteers meet these criteria, researchers can better understand results of the clinical trial.
Informed consent is a critical step before someone eligible can volunteer to participate in a clinical trial. The researcher will have a discussion with the participant to ensure they understand the details of the trial, what to expect before, during, and after, and what their rights are during the trial.
Clinical Trials Process
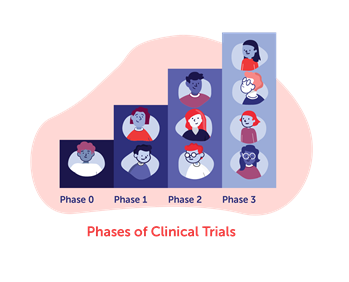
Clinical trials research the way a drug or treatment will interact with the human body and are conducted in phases. They play an important role in finding treatments that are safe and effective. Each phase is helping answer more questions to better understand the treatment. Some parts of the processes may differ in a gene or cell therapy clinical trial compared to other types of research for standard medical treatments.
Safety is a priority in each phase. If a study is not deemed safe, it will not move on to the next phase. This includes monitoring for adverse events, which are any unexpected health problems that might occur. The researcher collects information on whether the event relates to the treatment, the severity, frequency, and how to resolve it. In turn, these become the expected side effects to be aware of.
-
Phase one within most clinical trials tests if the treatment is safe for a small number of healthy volunteers. In gene and cell therapy clinical trials, the treatment can be far more risky and very specific to a disease, so healthy participants are not usually used. They will instead perform the tests on a small number of individuals with the disease. Sometimes this phase can determine the right dosage (amount of treatment given).
-
Phase two for gene and cell therapy trials expands the number of participants receiving the treatment, while other types of trials would now see if the treatment is safe in participants who have the disorder and further determine proper dosage. Both processes are looking to see if the benefits continue to outweigh risks.
-
Phase three typically lasts the longest. In this phase, the main goal is to see if the treatment gives the desired result while being safe in an even larger group of participants with the disorder of interest.
Phases can be combined to make the evaluation process more efficient. This is sometimes done for serious and rare diseases for which there is a clear unmet medical need, meaning a disease whose treatment or diagnosis is not addressed adequately by available therapy or if the treatment is too risky to test in a group of healthy volunteers. Gene and cell therapy clinical trials are often structured as a phase I / II study where a small group of participants with the disease are enrolled and both safety and efficacy tests are performed. There are some challenges to making this process shorter. Researchers need to avoid giving multiple patients too low of a dose to work or a dose so high it causes severe side effects. They also need enough time to fully assess the results of a trial whether benefits outweigh risks. It all goes back to making sure that the treatment is well understood, and safe and effective enough to be approved for the broader disease population.
A Biologics License Application (BLA) is submitted to the FDA if the results of the final phase of the clinical trial show the treatment to be safe and effective. Following careful review, the FDA makes a final decision about whether the treatment will be approved to use. This is when a treatment becomes “FDA approved” and is made more widely available to the intended patient population.
Patient Access
 Once a treatment successfully passes through clinical trials and is approved by the FDA, how can the people who are eligible access it?
Once a treatment successfully passes through clinical trials and is approved by the FDA, how can the people who are eligible access it?
Available at specialized sites. Currently, FDA-approved gene therapies are offered at a limited number of sites. These sites are academic medical centers with providers that are specially trained and experienced at giving the treatment.
Talk with a trusted healthcare provider. It’s important to inform your healthcare provider about potential clinical trial participation. You may also reach out directly to a medical center that offers the therapy. A trusted provider or member of the research team should help answer questions and ensure you understand any potential risks and unknowns, and consider the post-procedure care plan.
Check insurance coverage. The currently available gene therapies are covered by many health insurance options. Interested patients should contact their health insurance provider to determine their coverage and what to expect for out-of-pocket costs. Manufacturers of the gene therapies often offer patient support services to assist in the process Many patient advocacy groups are often supporting people in this part of the process as well.
Finding a Clinical Trial
 Participating in clinical trials is a way to receive an investigational product, while moving along research to help others who have the same disease or condition. If you are considering a clinical trial here are some steps you can take to access them:
Participating in clinical trials is a way to receive an investigational product, while moving along research to help others who have the same disease or condition. If you are considering a clinical trial here are some steps you can take to access them:
-
Explore the ASGCT Clinical Trials Finder to search for open clinical trials in gene and cell therapy. Search all ongoing clinical studies on ClinicalTrials.gov.
-
Talk to your doctor. Even if you find a clinical trial on your own, it is still important to talk with your doctor about it.
-
Sign up for a patient registry. Patient registries are a collection of information about patients who share a condition or experience. The goal is to help medical researchers better understand how diseases develop and progress over time. Some registries invite people to sign up to be contacted about participating in clinical research. Here’s a helpful list of patient registries from the National Institutes of Health (NIH), along with the National Organization for Rare Disorders (NORD) Registry Program, the Coordination of Rare Diseases at Sanford (CoRDS) and the Rare Diseases Registry Program (RaDaR).
-
Connect with patient organizations. Organizations such as NORD and Global Genes, or patient groups for specific diseases are a great place to start. They are hard at work to support rare genetic diseases and can be a great way to get updates and advocate for disease research.
FDA Efforts
The process of preclinical study and clinical trials take many years to conclude. Clinical trials alone sometimes take eight years or more. There are many factors that go into that duration including study planning, authorization to run a trial, ethics review, funding, research materials such as patient information, consent forms, and monitoring systems. However, FDA provides various expedited pathways (Fast Track, Breakthrough Therapy, Regenerative Medicine Advanced Therapy, Accelerated Approval, Priority Review) to accelerate the process for therapies that meet certain criteria while still maintaining safety.
Next, visit Gene Therapy Basics to learn more about how gene therapy works. Then review the Disease Treatment units to learn which disorders have approved therapies, and the potentials for treatments for other diseases.
Was this information helpful? If so, please share! All ASGCT Patient Education resources are free to use by sharing on social media, embedding the video, or simply linking to this page! Please credit The American Society of Gene and Cell Therapy.