UPDATE: On Friday, Dec. 8, 2023, the FDA approved two cell-based gene therapies, Casgevy and Lyfgenia, to treat sickle cell disease (SCD) in patients 12 years and older. These treatments are the first gene therapies approved for SCD in the U.S. and Casgevy is the first approved therapy in the U.S. that uses CRISPR. Learn more on our blog.
Sickle cell disease (SCD) is an inherited blood disorder that causes red blood cells to deform and become sickle (or crescent) shaped. These misshapen blood cells clump together and get stuck in blood vessels, blocking blood flow and depriving tissues and organs of oxygen-rich blood. This leads to a variety of problems including severe pain (also known as vaso-occlusive events), infections, organ damage, and can lead to premature death. Gene therapy and gene editing may offer a one-time treatment that addresses the genetic cause of sickle cell disease.
CASGEVY is an FDA-approved gene therapy for the treatment of individuals 12 years of age and older with sickle cell disease.
LYFGENIA is an FDA-approved gene therapy for the treatment of individuals 12 years and older with sickle cell disease.
About Sickle Cell Disease
Sickle cell disease occurs when a person inherits a faulty beta-globin gene, also known as the HBB gene. In adults, this gene controls how red blood cells produce hemoglobin, a protein that helps red blood cells carry oxygen throughout the body. Without enough functional hemoglobin, the red blood cells become stiff and take on a sickle shape. This causes the red blood cells to break apart easily, which leads to inflammation and damage to the blood vessels. The symptoms can impact a person’s everyday life by limiting their ability to do regular activities and can result in frequent hospital visits.
While in the womb, humans produce fetal hemoglobin, which comes from a different gene than the adult form. Typically, the fetal hemoglobin gene switches off shortly after birth. While most people switch to making healthy adult hemoglobin during infancy, people with sickle cell disease transition to making the abnormal form of adult hemoglobin because of the mutation in their HBB gene.
Gene Therapy Approaches
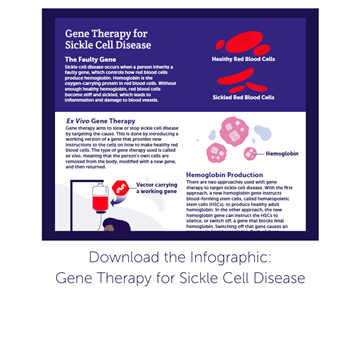
The gene therapy approach used is ex vivo, which means cells are removed from the body, modified with new genetic instructions, and then returned to the body to begin producing healthy blood cells. Chemotherapy is administered before gene therapy, as it eliminates existing stem cells that are still carrying the faulty gene. The cells removed from the body (through a blood draw) are hematopoietic stem cells, or HSCs, which are versatile cells that can turn into any type of blood cell the body needs. In one approach, referred to as gene addition, the HSCs can be instructed to produce more healthy adult hemoglobin by delivering (or adding) a working HBB gene. In another approach, referred to as gene silencing, a gene would be delivered that silences the BCL11A gene (or prevents it from working. The BCL11A gene typically acts as an “off” switch in our body and stops production of fetal hemoglobin after we are born. Silencing this gene allows the body to once again produce fetal hemoglobin. Fetal hemoglobin is similar to healthy adult hemoglobin in that it is able to carry oxygen effectively in the red blood cells to the tissues.
Learn more about using viral vectors in Vectors 101.

Gene Editing for Sickle Cell Disease
Gene editing is a type of gene therapy that removes, disrupts, or corrects faulty elements of DNA within a gene by using an enzyme that cuts the DNA at one specific location. The specific DNA cut allows changes to the sequence with high precision. There are various gene editing technologies under research, including ZFNs (zinc finger nucleases), and CRISPR-Cas variants (clustered regularly interspaced short palindromic repeats and CRISPR-associated protein 9.
As an example, the CRISPR-Cas9 system is a type of gene editing approach in which a small piece of RNA is created in a lab and attached to an enzyme (in this case, an enzyme called Cas9). The piece of RNA attaches to the target sequence of DNA, and the Cas9 enzyme will then cut the cell's DNA at that targeted location. Researchers have added a new piece of DNA that instructs cells to function properly.
Similar to the gene addition and gene silencing approaches, gene editing removes from the body hematopoietic (blood-forming) and progenitor cells (cells that give rise to mature cells). Then gene editing technology is used to either edit a portion of the BCL11A gene, which acts as the “off” switch to fetal hemoglobin production, or to directly edit the faulty HBB gene that causes sickle cell disease. The edited cells are then infused back into the patient as part of a stem cell transplant, helping them produce normal adult hemoglobin or fetal hemoglobin.
FDA-Approved Gene Therapies
CASGEVY is a CRISPR/Cas 9 based one-time cell-based gene therapy given for the treatment of individuals 12 years of age and older with sickle cell disease who:
Learn more about this type of therapy in Gene Editing.
LYFGENIA is a one-time cell-based gene therapy utilizing a lentiviral vector for the treatment of individuals 12 years and older with sickle cell disease who:
Learn more about lentiviral vectors in Vectors 101.
Other treatment options: A bone marrow transplant is a one-time, potentially curative option for sickle cell disease. However, less than one quarter of people with the disease are eligible for these transplants, as they would need to have a matching donor. The bone marrow transplant procedure and the medical care that follows it have potential complications, including infection and organ damage. To find out more visit the National Marrow Donor Program. Alternatively, pain relievers or blood transfusions can help manage the symptoms of sickle cell disease. Blood transfusions are typically administered once or twice a month for people with the disease. In contrast, gene therapy uses the person's own cells, eliminating the need for a donor while treating the cause of the disease. Gene therapy aims to be administered only once and has the potential to be curative.
Treatment Pipeline
Further gene therapy and gene editing approaches are being researched in trials for SCD. Clinical trials are a required part of the research process that aims to understand the way a drug or treatment will interact with the human body and whether it is safe and effective. Preclinical studies are an even earlier stage of research to confirm the safety and effectiveness of a treatment in animal or cell-based models before proceeding with a human clinical trial. Clinical trials may differ on various aspects of their design. Speak with a trusted provider or member of the clinical trial research team if you are considering participating in a clinical trial.
To stay up to date on active and recruiting clinical trials that may become available in the U.S. or globally, visit ClinicalTrials.gov or the Gene Therapy Trial Browser.
Participating in a Clinical Trial
It is important to be well informed when deciding to participate in a clinical trial. Below are some key points to consider. Visit the considering a clinical trial page for more information and resources to help guide you.

-
Eligibility - Eligibility for a trial is based on strict inclusion and exclusion criteria. These are specific factors that determine whether a person can or cannot enroll in a clinical trial. This is an important way for researchers to understand if the gene therapy is working properly and to ensure participant safety. These criteria may include factors such as age, physical ability, medical history, and more. Speak with a healthcare provider or a member of the clinical trial research team to help determine if you or your child may be eligible for a clinical trial. These criteria usually include age—typically the minimum age for participants is 18 and the maximum is 40 years old for sickle cell disease trials. Also, medical history is important to consider. Many clinical trials require participants to have no history of gene therapy treatment or organ transplants, and their sickle cell disease must be considered “severe.”
-
Risks - As with any medical intervention, there are risks that need to be carefully considered. Before participating in a clinical trial, a member of the research team should review any potential risks and benefits with the patient or caregiver. Therapies being studied in clinical trials are not a guaranteed cure and cannot guarantee beneficial results. There is always a chance that the investigational treatment may not work. In the event a person is not satisfied with the outcome, the person may not receive another dose of the gene therapy. In addition, participating in a clinical trial may prevent future participation in other trials or from receiving other types of treatments. Gene therapy can be an alteration for the lifetime, so people should be aware that there could be long term effects (both good or bad) that are not known at this time.
-
Benefits - Participating in a trial may offer many potential benefits compared to not receiving any form of intervention for a fatal disease. Gene therapy aims to be a one-time treatment with lasting positive effects that slow or stop disease progression for a lifetime. However, there is no guarantee. If gene therapy is received earlier in the course of disease, it has the potential to stop damage before it occurs.
-
Long-term follow up - It is the patient’s responsibility to comply with the long-term follow-up of a trial. The Food and Drug Administration (FDA) guidelines require the clinical trial research team to monitor safety and potential long-term effects of a gene therapy. Follow-up may require in-person appointments that vary in frequency and location, or completion of mailed packets with response forms. The need for long-term data collection for a gene therapy trial can last up to 15 years—another reason to consider all outcomes and responsibilities that come with committing to a clinical trial. There are a limited number of participants in trials so a lack of attendance at follow-up appointments leads to not enough study data. This could negatively affect FDA approval of a new therapy and thereby limit access to the therapy by patients who did not participate in the clinical trial.
Access
At this time, we do not know if or when more gene therapies will be approved by the FDA and commercially available for people living with Sickle Cell Disease. The overall process may take several more years, until it is deemed safe and effective by the FDA or regulatory agencies in other countries.
Get Involved
A number of organizations provide individuals affected by Sickle Cell Disease, and their families, with resources, research updates, and support: